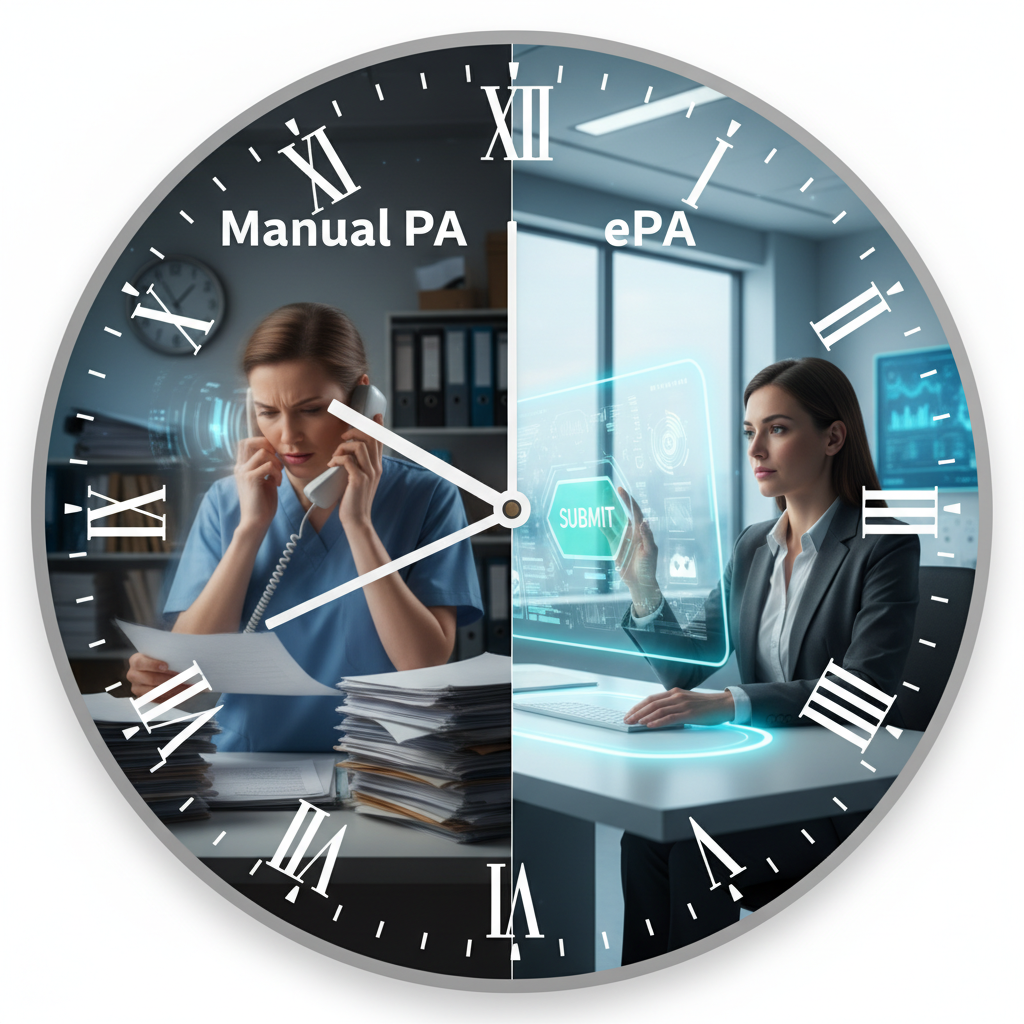
Prior authorization (PA) has long been a source of friction in healthcare. It’s a process intended to manage costs and ensure appropriate care, but it often results in administrative headaches, treatment delays, and frustration for providers and patients alike. The manual nature of traditional PA—involving phone calls, faxes, and navigating various payer portals—consumes valuable resources and can negatively impact patient outcomes.
Fortunately, the shift toward electronic prior authorization (ePA) is transforming this landscape. By leveraging technology to automate and standardize the authorization process, ePA offers a clear path to greater efficiency, reduced administrative burden, and faster access to care. This transition is no longer a distant goal; it’s a present-day reality, accelerated by new federal regulations and proven technological solutions.
This guide explores the challenges of manual PA, the regulatory push for electronic systems, the significant benefits of ePA for both providers and patients, and the technologies making it all possible. Understanding these elements is crucial for any healthcare organization looking to streamline its operations and improve patient care.
The Problem with Manual Prior Authorization
The manual prior authorization process is a well-documented pain point for the healthcare industry. For clinicians, it’s a time-consuming administrative task that detracts from patient care. For patients, it can become a barrier to receiving necessary treatments, leading to delays that can have serious clinical consequences.
Administrative Burdens and Inefficiencies
The administrative load associated with manual PA is staggering. Healthcare providers spend an average of 15 hours per week managing authorization requests. This burden is spread across a fragmented system of different communication methods, including phone calls, faxes, and insurer-specific web portals. Because every insurer has its own unique forms, coding rules, and documentation requirements, clinical staff must constantly adapt their workflow, creating significant inefficiencies.
This lack of standardization means there is often no single, streamlined workflow for processing prior authorizations within a provider organization. Staff must manually abstract clinical data from a patient’s medical record, often as a PDF, and upload it to the correct payer portal. This process is not only labor-intensive but also prone to human error, which can lead to further delays.
Delays and Denials Impacting Patient Care
These administrative hurdles directly translate into delays and denials that affect patient care. According to the American Medical Association (AMA), prior authorization delays impact patient care in over 90% of cases. The introduction of a new PA requirement for an established drug, for example, has been shown to increase the odds of a patient discontinuing their medication by more than sevenfold. The time to the next fill also increases by an average of 9.7 days.
Such gaps in care are concerning for any condition but can be particularly risky for patients relying on time-sensitive treatments, like oral anticancer drugs, where adherence is critical to prevent acquired drug resistance. A primary reason for denials is often a lack of sufficient clinical documentation. Even when the information exists, the cumbersome manual process of submitting it can cause bottlenecks, resulting in postponed treatments and patient dissatisfaction.
The Human and Financial Cost
The inefficiencies of manual PA carry a significant financial cost for healthcare organizations. The time spent by clinical and administrative staff on these tasks represents a major operational expense. Beyond the direct labor costs, delays can lead to patients abandoning recommended treatments, which not only affects their health but can also have downstream financial implications for the healthcare system.
At Midwest Family Clinic in Ohio, an internal audit revealed that 40% of their PA delays were due to incomplete paperwork and a lack of follow-up. This is a common scenario that highlights how manual processes contribute to physician burnout, suboptimal patient experiences, and a strained healthcare workforce.
The CMS Push Toward Electronic Systems
Recognizing the significant burdens of manual prior authorization, regulators have taken decisive steps to accelerate the adoption of electronic systems. The Centers for Medicare & Medicaid Services (CMS) is at the forefront of this movement, issuing rules that mandate a shift toward a more streamlined, transparent, and efficient process.
New Federal Mandates for ePA
A pivotal CMS rule is set to bring major changes by 2026 and 2027. This rule places new requirements on Medicare Advantage organizations, state Medicaid and CHIP programs, and other health plans to implement electronic prior authorization processes. The goal is to create a more interconnected and responsive system that reduces the administrative load on providers and speeds up care delivery.
Key provisions of the CMS rule include:
- API for Authorization: By January 1, 2026, payers must implement a Fast Healthcare Interoperability Resources (FHIR)-based API. This will allow provider systems to electronically determine if an item or service requires prior authorization and to submit and track requests.
- Decision Timelines: Payers will be required to provide PA decisions within 72 hours for expedited requests and seven calendar days for standard requests.
- Denial Reasons: When a request is denied, payers must provide a specific reason to the provider, improving transparency and facilitating appeals.
- Public Reporting: Beginning in March 2026, insurers will be required to publicly report certain PA metrics, such as approval and denial rates, offering greater insight into their processes.
Several states have also passed их own legislation requiring ePA, reinforcing the national trend toward digitalization. While these deadlines may seem distant, forward-thinking organizations like Ochsner Health are already well on their way to meeting these requirements, demonstrating the feasibility and benefits of early adoption.
Adopting Technical Standards
To facilitate this electronic transition, CMS has adopted technical standards for ePA transactions. The established standard is the HIPAA X12 278, which handles health care service review requests and responses. However, its adoption has been limited, with only 31% of PA transactions using this standard in 2023.
To encourage broader interoperability, CMS has also provided an exception for the use of HL7 FHIR-based API standards developed by initiatives like the Da Vinci Project. These newer, more flexible standards are designed to better integrate with modern electronic health record (EHR) systems, allowing for a more seamless exchange of information between providers and payers. The ultimate aim is to create a single, standardized workflow that works across all payers, eliminating the need for providers to navigate multiple disparate systems.
Read More: Regulatory Shifts in Medical Billing 2025: ICD-11, E/M Coding, Telehealth & What Providers Must Know
Benefits for Providers and Patients
The transition to electronic prior authorization offers transformative benefits for मूडь healthcare providers and the patients they serve. By automating and streamlining a historically manual process, ePA directly addresses the core pain points of cost, delay, and administrative burden.
For Healthcare Providers
For providers, the most immediate benefit is a dramatic reduction in administrative workload. Integrating ePA workflows directly into the EHR means staff no longer need to log into multiple payer websites or spend hours on the phone. At Ochsner Health, which began implementing ePA several years ago, the preservice and authorization teams now work exclusively within their Epic EHR to communicate with payers.
This streamlined process delivers tangible results:
- Time Savings: Ochsner Health has saved hundreds of staff hours, a number expected to grow into the thousands. Across the country, clinics that centralize their PA work and use standardized electronic forms have cut staff time per request by 30-60%.
- Increased Efficiency: With ePA, routine authorizations can be completed in hours instead of days or weeks. For common drugs and basic scans that fit established rules, approvals can even be instantaneous. Ochsner Health reports receiving instantaneous approvals about half the time through their EHR platform.
- Lower Denial Rates: A leading cause of PA denials is missing clinical documentation. ePA systems allow providers to send this data directly from the EHR to the payer, either upfront or immediately upon request. This has been shown to decrease denial rates, as providers can more easily supply the necessary evidence to support their requests.
- Improved Staff Satisfaction: By removing cái tedious and frustrating aspects of manual PA, ePA has been “incredibly transformative” for the staff who manage these tasks daily. This allows them to focus on more complex cases and higher-value work.
For Patients
Ultimately, the most important benefits are those experienced by patients. When the authorization process is faster and more efficient, patients can access the care they need without unnecessary delays.
- Faster Access to Care: The time to get an answer on a prior authorization request has shrunk from days or weeks to mere hours or days. This means patients can start their treatments sooner, which is especially critical for time-sensitive conditions.
- Reduced Treatment Abandonment: By simplifying the authorization process, ePA reduces the chances that a patient will abandon their recommended treatment due to administrative hurdles. This is particularly important for patients on established drug regimens, where continuity of care is vital.
- Greater Transparency: ePA systems can provide patients with greater visibility into the status of their authorization requests. This transparency helps manage expectations and reduces the anxiety associated with waiting for approvals.
By ensuring care is delivered “faster, more efficiently, and more appropriately,” as one expert from Ochsner Health noted, ePA delivers a clear win for patient outcomes and satisfaction.
The Technology Solutions Driving ePA
The successful implementation of electronic prior authorization hinges on a new generation of technology solutions designed to bridge the gap between providers and payers. These tools leverage interoperability standards, API integrations, and artificial intelligence to automate and streamline workflows.
Interoperability and Standardized APIs
At the core of modern ePA are standardized application programming interfaces (APIs) built on frameworks like HL7 FHIR. These APIs act as a universal translator, allowing different systems—such as a provider’s EHR and a payer’s management system—to communicate seamlessly. The Da Vinci Project has been instrumental in creating FHIR-based APIs specifically for prior authorization, facilitating the electronic exchange of health information.
This standardization is critical. It enables a “single workflow for all,” where providers can manage authorizations for multiple payers through one interface, typically embedded directly within their EHR. This integrated approach is already a reality for many, with over 200 organizations now exchanging data with 16 major payers, covering more than 100 million lives.
Integration with Electronic Health Records (EHR)
True efficiency is achieved when ePA tools are deeply integrated into the clinical workflow. By connecting directly to a provider’s EHR, these systems can pull necessary patient data, pre-populate forms, and submit requests without requiring staff to leave the application they use all day. This not only saves time but also reduces the risk of manual data entry errors.
Leading EHR providers like Epic are offering proprietary platforms that facilitate these connections. These “real-time EHR connectivity” frameworks embed near-real-time authorization functionality directly into the clinician’s workflow, delivering insights and actions at the right moment in the patient’s journey.
The Role of Artificial Intelligence (AI)
Artificial intelligence is poised to further revolutionize prior authorization. AI-powered tools can assist in several ways:
- Preparing Requests: AI can scan a patient’s medical record to identify key clinical details and flag any missing information needed for an authorization request. The final submission is still reviewed by a human, but the initial preparation is significantly accelerated.
- Automated Triage: For payers, AI can help automate the intake and triage of PA requests, standardizing clinical decision-making and improving the efficiency of the review process.
- Predictive Analytics: By analyzing historical data, AI can help predict the likelihood of an approval, allowing providers to focus their efforts on more complex cases that require manual intervention.
However, it’s important to approach AI with caution. Blind trust in automated systems can lead to unfair denials if not properly overseen. Effective implementation requires that staff always review AI-flagged decisions and that the tools are customized to account for each payer’s unique rules.

Read More: The Rise of AI in Healthcare: Smarter Triage and Faster Diagnoses
Your Next Steps Toward Streamlined Authorization
The shift from manual, burdensome prior authorization to a streamlined electronic process is no longer a future aspiration—it is a present-day imperative. Driven by regulatory mandates and enabled by mature technology, electronic Prior Authorization (ePA) offers a clear path to reducing administrative waste, cutting costs, and, most importantly, ensuring patients receive timely access to necessary care.
At Care Medicus, we specialize in guiding healthcare organizations through this critical transition. By embracing EHR-integrated tools, standardized APIs, and intelligent automation, we help you transform a process of frustration into a model of efficiency. This transition not only improves the bottom line and boosts staff morale but also delivers on the fundamental promise of healthcare: to provide the best possible care without unnecessary delay.
The time to begin this journey is now. Partner with Care Medicus to unlock the full potential of electronic prior authorization and build a future where administrative hurdles never stand in the way of patient health.






Leave a Reply