When healthcare systems operate in isolation, patient care suffers. Critical information gets trapped in data silos, leading to incomplete patient histories, redundant tests, and disjointed care coordination. This lack of connection, known as poor interoperability, doesn’t just frustrate doctors and patients; it costs the U.S. health system an estimated $30 billion annually.
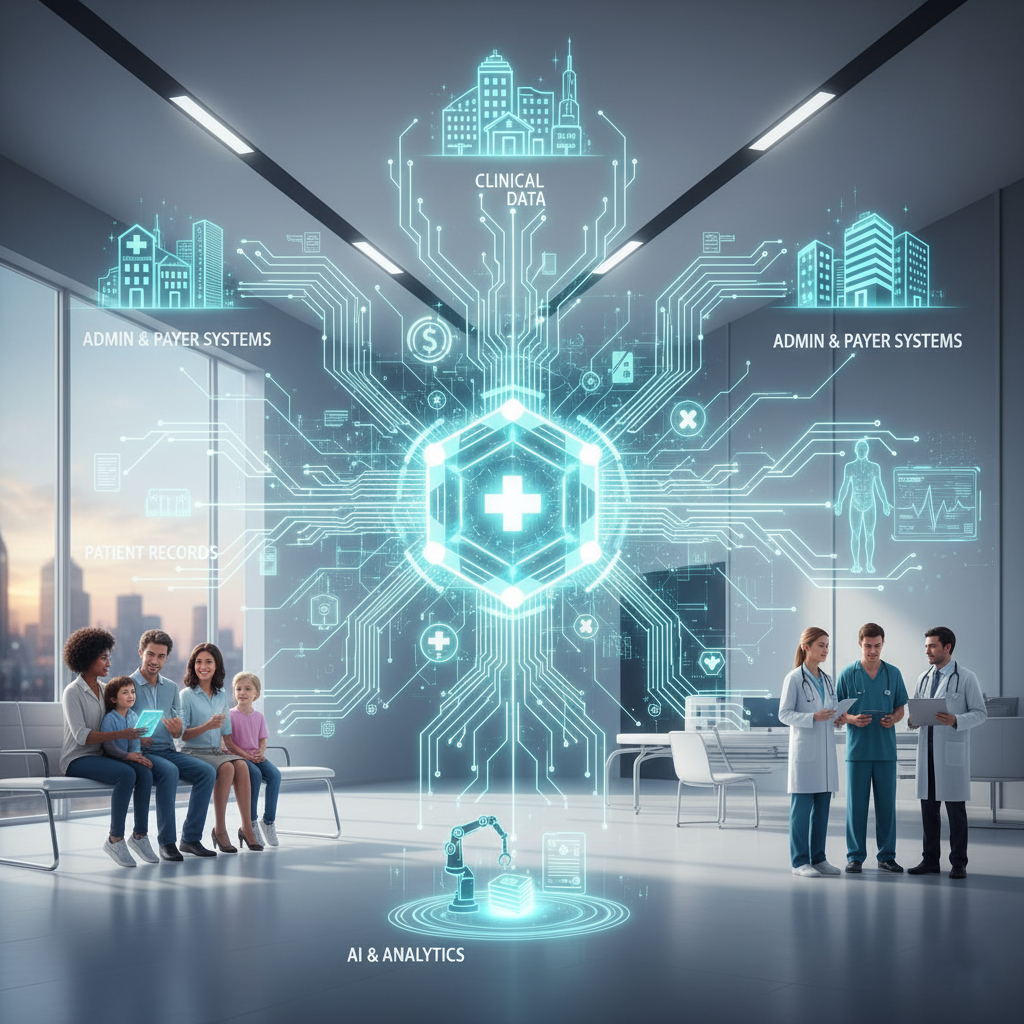
The solution lies in creating a connected healthcare ecosystem where different systems and devices can securely access, exchange, and use electronic health data. This is the core of interoperability. By enabling systems to “speak the same language,” we can empower medical professionals with the comprehensive, up-to-date information they need to provide the best possible care. This guide will explain what interoperability is, why it’s essential for modern healthcare, and the steps organizations can take to build a more connected future.
What is Healthcare Interoperability?
Interoperability in healthcare is the ability of different information technology systems and software applications to communicate, exchange data, and use the information that has been exchanged. The goal is to allow for the seamless and secure sharing of electronic health information between devices and systems without special effort from the user.
Ultimately, this means a patient’s complete health journey—from primary care visits to hospital stays and pharmacy records—is available for providers to analyze and act upon, leading to a holistic and continuous care experience.
The Four Levels of Interoperability
The Healthcare Information and Management Systems Society (HIMSS) outlines four distinct levels of interoperability, each building on the last to create a fully integrated system.
- Foundational Interoperability: This is the most basic level. It ensures that one system can securely send data to another. However, the receiving system doesn’t need to be able to interpret the data. Think of it as sending a sealed letter; the recipient gets the package, but can’t necessarily read what’s inside.
- Structural Interoperability: This level standardizes the format of the data exchange. It defines the structure and syntax of the data, ensuring that it can be interpreted by multiple systems. This is like ensuring everyone uses the same filing system, so data fields are consistent and recognizable.
- Semantic Interoperability: This is where systems not only exchange data but also understand its meaning. It involves the use of standardized terminologies (like SNOMED CT) so that concepts like “heart attack” are understood uniformly across different systems, even if they use different internal data structures.
- Organizational Interoperability: The highest level involves seamless data exchange between various organizations, often with different goals, regulations, and requirements. This includes governance, policy, and social considerations to support secure and reliable data sharing across institutional and jurisdictional boundaries.
The Transformative Benefits of System Integration
Achieving true interoperability is more than a technical exercise; it fundamentally transforms healthcare delivery for providers, payers, and patients. When systems are integrated, the entire healthcare ecosystem becomes more efficient and effective.
Better Care Coordination and Patient Outcomes
With a complete view of a patient’s medical history, providers can make more informed decisions, reduce medical errors, and avoid repeating expensive tests. A study found that 83% of health systems already use data from Health Information Exchanges (HIEs) to support patient care. This comprehensive patient view enables providers to deliver a holistic continuum of care, ultimately improving patient safety and health outcomes.
Increased Efficiency and Lower Costs
A significant portion of healthcare spending is lost to waste and administrative inefficiencies, much of which stems from the inability to share data. Interoperability streamlines workflows, automates tasks, and reduces the administrative burden on clinicians, allowing them to focus more on patient care. This not only improves efficiency but also helps reduce costs and can increase reimbursements in value-based care models.
Data-Driven Insights for Population Health
When data from disparate sources is combined and analyzed, healthcare organizations can uncover powerful insights into population health trends. This enables proactive health management, better resource allocation, and the development of targeted public health initiatives. It helps organizations maintain a competitive advantage by strengthening value-based care delivery and improving the overall quality of care.

Key Challenges on the Path to Interoperability
Despite clear benefits and strong government incentives like the 21st Century Cures Act, achieving widespread interoperability remains a significant challenge. Healthcare organizations face a combination of technical, financial, and organizational hurdles.
- Technical Barriers: Many healthcare providers still rely on legacy systems and data silos that were not designed to communicate with other platforms. Furthermore, data quality is a major issue, with reports indicating that 60% of health systems receive duplicate, incomplete, or “junk” data, while 69% receive incomplete data.
- Data Security and Privacy: The sensitive nature of health data makes security a top priority. Organizations must navigate strict privacy regulations like HIPAA while ensuring data can be shared securely. Concerns about patient privacy are a leading reason why full integration is not yet a reality.
- Financial Constraints: The cost of implementing new, interoperable systems can be substantial, particularly for smaller practices and startups. Although 55% of health system CIOs planned to increase spending on interoperability in 2023, budget limitations remain a significant barrier.
- Organizational Resistance: Change can be difficult. A lack of collaboration between departments, resistance from staff, and unclear governance can slow down or halt interoperability initiatives. For instance, 40% of surveyed EHR vendors are aware of the need to join a Qualified Health Information Network (QHIN) but are not prioritizing the action.
Building a Connected Future
Overcoming these challenges requires a strategic approach that combines technology, standards, and collaboration. Several key trends and solutions are paving the way for a more interoperable future.
Adopting Standards and APIs
Standards like Health Level Seven (HL7) and Fast Healthcare Interoperability Resources (FHIR) provide a common framework for exchanging healthcare information. FHIR, in particular, is an open-source framework that makes it easier for data to move between systems. The use of Application Programming Interfaces (APIs) allows different software applications to communicate and share data, breaking down the monolithic systems of the past.
Leveraging Cloud Technology and AI
Cloud-based solutions offer a scalable and secure way to store, share, and access patient data in real-time. When combined with strong encryption, cloud technology can address many security concerns. Furthermore, artificial intelligence (AI) and machine learning are being used to parse unstructured data, such as clinical notes, and convert it into a usable format. AI-based solutions can also help bridge the gap between modern technologies and legacy systems by improving data extraction and streamlining workflows.
Focusing on Data Quality
Harmonizing data and ensuring its accuracy is critical. Solutions that focus on data quality and semantics help ensure that the data being shared is reliable and meaningful. This step is essential for building trust in the exchanged information and making it clinically useful.
Your Next Steps Toward Integration
At Care Medicus, we believe that interoperability is not just an upgrade—it is the foundation of modern healthcare. The ability to exchange information seamlessly across systems is essential to improving patient outcomes, reducing costs, and empowering clinicians to deliver truly coordinated care.
Now is the time for healthcare organizations to take decisive action. Commit to breaking down data silos, adopt standardized data formats, and invest in interoperable technologies that connect every point of care. Partner with trusted innovators like Care Medicus to navigate the complexities of healthcare integration and drive measurable transformation.
Together, we can build a smarter, more connected healthcare ecosystem—one where every piece of information serves its highest purpose: improving lives.





Leave a Reply