Pathology has long been considered the “canary in the coal mine” for revenue cycle management (RCM). Because high-volume, low-dollar tests make up the bulk of clinical pathology revenue, even small shifts in payer policies can trigger massive financial tremors. A denial rate increase of just 2% might be negligible for a surgery center, but for a lab running thousands of automated panels a week, it can wipe out margins entirely.
As we move into 2026, the canary is gasping. Payers are deploying increasingly sophisticated algorithms to flag what they consider “excessive” testing. The days of flying under the radar with standard panels are over. The new battleground is defined by frequency caps and intense scrutiny on Modifier 91—the mechanism used to bill for repeat tests.
For labs and pathology groups, the trap is set. Legitimate medical necessity often clashes with rigid automated payer edits, leading to a surge in denials for tests like lipids, TSH, and hormones. Escaping this trap requires more than just submitting claims; it demands a strategic overhaul of how clinical pathology is documented, coded, and appealed.
The 2025 Scrutiny: Why High-Volume Tests Remained Under Attack
The landscape of clinical pathology billing is shifting beneath our feet. In previous years, audits were typically reserved for high-cost genetic testing or complex molecular diagnostics. Today, the focus has broadened to include the “bread and butter” of the lab: high-volume, automated chemistry and hematology tests.
Why the shift? It comes down to volume and automation. Insurance companies have realized that by implementing strict frequency edits on common tests, they can save millions in aggregate costs.
The Targets: Lipids, TSH, and Hormones
Specific test codes are currently triggering audits at an unprecedented rate. These include:
- Lipid Panels (CPT 80061): Payers are increasingly enforcing guidelines that limit lipid screening to once a year for low-risk patients, despite clinical realities that might require more frequent monitoring for patients on statin therapy.
- Thyroid Stimulating Hormone (TSH – CPT 84443): While essential for titrating thyroid medication, consecutive tests performed too close together are being automatically flagged as duplicates or medically unnecessary.
- Hormone Panels: Tests for testosterone, estradiol, and other hormones are facing stricter “medical necessity” criteria, particularly when ordered as part of wellness or anti-aging protocols rather than for diagnosing specific pathology.
The result is a landscape where clinical validity does not guarantee payment. A physician may have a perfectly valid reason for ordering a repeat test, but if the billing data doesn’t explicitly bridge the gap between the clinical need and the payer’s algorithm, the claim will die in the clearinghouse.

The Modifier 91 Mystery: Navigating the “Repeat Test” Minefield
At the heart of many of these denials lies Modifier 91. This two-digit appendage is designed to tell the payer: “This is not a duplicate error. We meant to run this test again on the same day.”
However, Modifier 91 has become an audit magnet. Payers have trained their systems to view Modifier 91 with suspicion, often assuming it is being used to bypass duplicate edit checks (NCCI edits) rather than to report a legitimate clinical event.
When to Use Modifier 91 (And When to Walk Away)
Misuse of this modifier is rampant, often due to confusion with Modifier 59 (Distinct Procedural Service). To survive audits in 2025, billing teams must strictly adhere to the appropriate usage guidelines:
- Same Patient, Same Day, Same Test: Modifier 91 is only for when the exact same CPT code is performed on the same patient on the same date of service.
- New Specimen Required: It generally implies a new specimen was collected at a different time (e.g., assessing potassium levels in the morning and again in the afternoon to monitor treatment).
- Medical Necessity is Key: It cannot be used to confirm results or because of a lab error. If the machine malfunctioned and you re-ran the test, you cannot bill for it twice.
The “Duplicate” Trap
The most common denial reason associated with Modifier 91 is “Duplicate Service.” Even when the modifier is applied correctly, payers’ automated systems often ignore it on the first pass.
Example:
A diabetic patient in ketoacidosis has their glucose checked at 9:00 AM, 12:00 PM, and 3:00 PM.
- Test 1: 82947 (Glucose)
- Test 2: 82947-91
- Test 3: 82947-91
If the diagnosis codes for Tests 2 and 3 don’t specifically support the need for serial monitoring (e.g., E11.10 Type 2 diabetes with ketoacidosis), the payer’s computer sees three glucose charges and denies two of them as duplicates. The modifier alone is often not enough; the diagnosis pointers must scream “acute change in condition.”
Read More >> Beyond the Appeal: Building an “Autonomous” Denial Prevention Strategy
The Documentation Gap: Where Revenue is Lost
The root cause of most pathology denials isn’t usually in the lab—it’s in the physician’s notes. There is a widening chasm between the results the lab produces and the “medical necessity” documented in the electronic health record (EHR).
Pathologists and lab directors rarely see the patient. They rely on the ordering physician to provide the diagnosis codes (ICD-10). Unfortunately, physicians often select a generic code that justifies the visit but not necessarily the frequency of the lab test.
Connecting the Dots
To solve this, RCM teams must bridge the gap between the lab information system (LIS) and the ordering provider’s data.
- Specific vs. Generic ICD-10: A claim for a repeat TSH test submitted with “Unspecified Hypothyroidism” is a candidate for denial if billed twice in three months. A claim submitted with codes indicating “drug titration” or “abnormal findings” has a much higher survival rate.
- The “Rule Out” Problem: Labs cannot bill based on a “rule out” diagnosis. If a doctor orders a panel to rule out a disease, and the result is negative, the coding must reflect the symptoms that prompted the test, not the condition that wasn’t found.
- Access to Clinical Notes: In an audit, the payer requests the medical record. If the lab does not have access to the physician’s notes proving why a repeat test was needed at 2:00 PM, the appeal is lost before it begins.
Frequency Caps: Strategies for the “2x Per Year” Limit
One of the most frustrating challenges in 2025 is the hard frequency cap. Many commercial plans have instituted policies limiting certain tests (like Vitamin D or Lipid Panels) to a specific number per year—often just once or twice—regardless of the diagnosis.
When a patient hits this cap, the claim is rejected with a message stating “benefit maximum has been reached.” However, these caps are rarely absolute; they are usually “soft” caps that can be overridden with specific medical necessity proof.
Managing the Cap
- Advance Beneficiary Notice (ABN) Management: For Medicare patients, knowing frequency limits is vital for issuing ABNs. If you know a test is likely to be denied for frequency, obtaining a signed ABN allows you to bill the patient. Without it, the lab eats the cost.
- Commercial Waivers: For private payers, “soft” caps can often be bypassed if the patient has a specific high-risk diagnosis. For example, a patient with a history of cardiovascular disease is often exempt from the “one lipid panel per year” rule. The billing system must be sophisticated enough to recognize high-risk ICD-10 codes and prioritize them on the claim form.
- Historical Data Analysis: Labs should run reports on their top denial codes. If CPT 80061 is being denied for frequency in 15% of cases, it signals a need to update the front-end rules engine to check patient history before the specimen even hits the analyzer.
Automation in the Lab: Fighting Algorithms with Algorithms
If payers are using AI to deny claims, labs must use AI to get them paid. The volume of clinical pathology makes manual review of every claim impossible. The solution lies in automation that occurs before the claim is submitted.
Cross-Referencing CPT Codes with Clinical Justification
Modern RCM platforms can now integrate directly with the LIS to perform real-time scrubbing.
- Modifier Logic: AI tools can scan a batch of claims, identify same-day duplicates, and automatically append Modifier 91 only when the time stamps and test types align with NCCI guidelines.
- Diagnosis Matching: Automation can flag orders where the provided ICD-10 code does not meet the Local Coverage Determination (LCD) or National Coverage Determination (NCD) criteria for medical necessity. This allows the billing team to query the provider for a more specific code before the denial happens.
- Denial Prediction: Machine learning models can analyze payer behavior to predict which claims will hit a frequency cap. If a Blue Cross plan in a specific state has started denying Vitamin D tests for code Z00.00 (General Exam), the system can flag these claims for manual review or updated coding.
Read More >> AI and Predictive Analytics in Healthcare to Reduce Claim Denials
Conclusion: Protecting Lab Margins in an Era of Decreasing Reimbursement
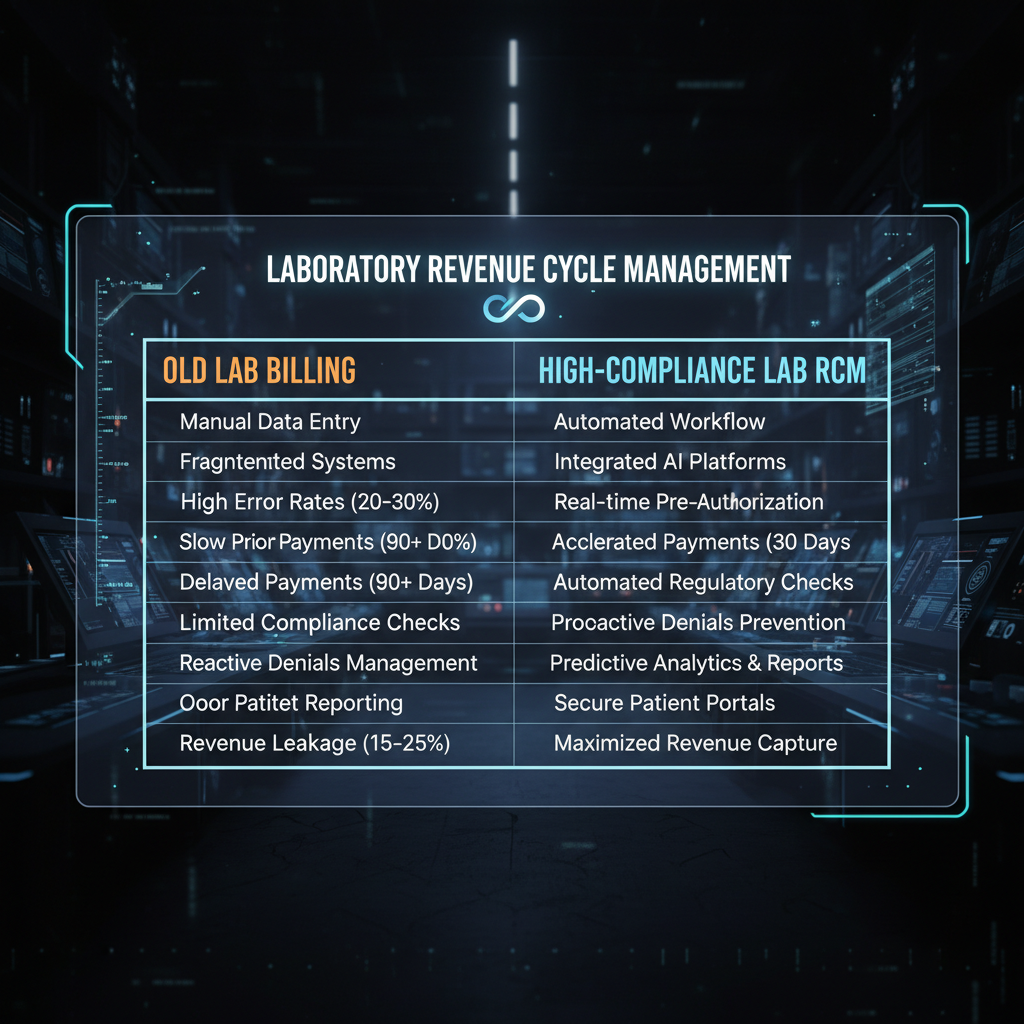
The pressure facing clinical pathology labs is not easing—it’s intensifying. Shrinking reimbursements, expanding administrative demands, and heightened scrutiny around frequency caps and Modifier 91 have created an environment where getting paid is often harder than delivering the science itself. At Care Medicus, we understand that these payer strategies are designed to reduce spend, frequently at the expense of laboratory sustainability.
But this challenge is not inevitable. Labs that move away from reactive, “spray and pray” billing practices and adopt a data-driven, compliance-first revenue cycle strategy can protect margins and regain control. Success begins with education—ensuring teams clearly understand the distinction between duplicate billing errors and legitimate repeat procedures. It continues with integration—breaking down silos between laboratory data and ordering physician documentation so medical necessity is indisputable. And it is sustained through automation—using technology to scrub claims against payer-specific frequency rules before submission, not after denial.
The labs that will thrive in 2026 will not be defined by science alone, but by operational intelligence. With deep expertise in laboratory revenue cycle management and compliance-driven automation, Care Medicus helps pathology organizations build smarter billing frameworks that reduce denials, withstand payer scrutiny, and secure rightful reimbursement the first time.
The rules may keep tightening—but with the right strategy, your lab doesn’t have to absorb the cost.






Leave a Reply