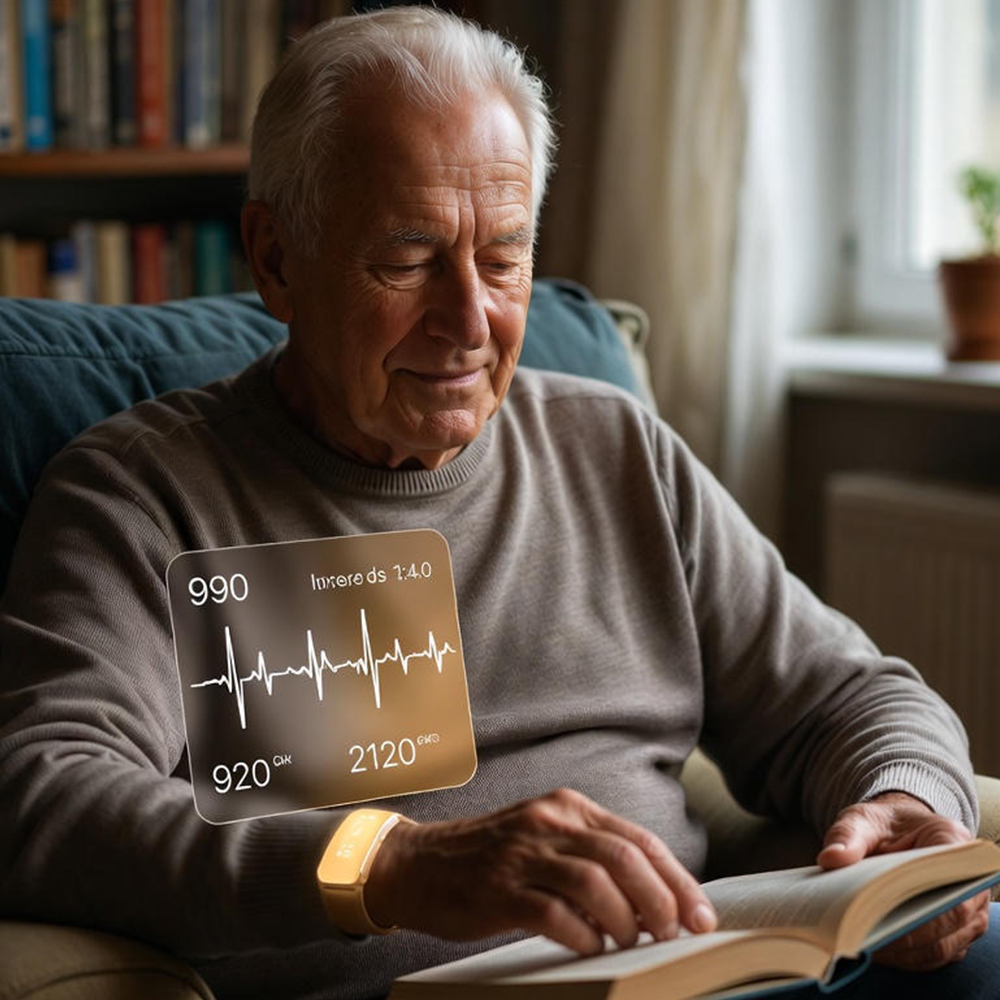
Imagine recovering from a major cardiac event, not in a sterile room filled with the beep of monitors and the smell of antiseptic, but in your own bed. You are surrounded by family, eating home-cooked meals, and resting with your pets nearby. In the past, this scenario was a trade-off: you gained comfort but lost the rigorous safety net of 24/7 observation.
That dynamic has fundamentally shifted. The walls of the traditional hospital are dissolving, replaced by a sophisticated digital infrastructure that makes the home environment not just comfortable, but clinically precise.
The old model of at-home care failed for high-acuity patients because it was reactive. It relied on scheduled manual check-ins, phone calls, and the patient’s own ability to recognize when something was wrong. By the time a patient felt sick enough to call for help, the window for early intervention had often closed.
Today, we are witnessing a paradigm shift. Powered by predictive AI and advanced remote patient monitoring (RPM), home-based care is no longer a “lesser” version of inpatient treatment. When backed by predictive analytics, the home becomes potentially the safest place on earth for recovery.
Mission Control: The AI-Driven Dashboard
To understand how high-risk care can happen in a suburban living room, you first have to look at the “Command Center.” This isn’t located in the patient’s house, but in a centralized hub where a specialized team of clinicians manages hundreds of virtual beds simultaneously.
This Command Center functions like air traffic control for healthcare. Instead of tracking planes, they are tracking patient stability. But unlike a traditional hospital ward where a nurse must walk from room to room to check vitals, the data here flows continuously.
Visualizing the Tech
The heart of this system is the AI-driven dashboard. It aggregates real-time data from a suite of connected devices—continuous glucose monitors, pulse oximeters, smart beds that track respiration during sleep, and ambient sensors that detect falls or changes in gait.
However, data without context is just noise. If a nurse had to manually review thousands of data points per minute for hundreds of patients, the system would collapse. This is where artificial intelligence steps in.
The dashboard utilizes a color-coded triage system. The AI analyzes the data stream and assigns a “Risk Score” to every patient:
- Green: The patient is stable and recovering as expected.
- Yellow: There are minor deviations from the baseline that require observation.
- Red: The patient is deteriorating or at immediate risk.
This system allows clinicians to filter out the noise. They don’t need to watch the stable patients; the system does that for them. Instead, the “Human-in-the-Loop” philosophy ensures that highly trained nurses and doctors focus their attention exclusively on the patients who need it most. The AI doesn’t replace the clinician; it acts as a super-powered lens, directing their eyes to the exact point of critical need.

Read More: Benefits of Cloud Based System in Healthcare
Predictive Triage: Catching the “Invisible” Decline
The true power of this technology lies in moving from reactive to predictive care. In a traditional setting, a “Code Blue” happens when a patient crashes. In an AI-enabled at-home care model, the goal is to intervene before the crash ever happens.
This is the science of forewarning. The human body rarely fails all at once; it gives subtle clues hours or even days before a major event. A 2% drop in blood oxygen saturation combined with a slight, gradual increase in respiratory rate might not look alarming on a standard chart. To a busy floor nurse, these might seem like normal fluctuations.
To a predictive algorithm, however, this pattern is a screaming siren. It recognizes these “micro-deteriorations” as the precursor to sepsis, heart failure decompensation, or respiratory distress.
The “Digital Twin” Concept
To make these predictions accurate, advanced systems utilize the concept of a “Digital Twin.” Upon admission to the virtual ward, the system creates a digital model of the patient based on their medical history, age, condition, and baseline biometrics.
The AI then constantly compares the real-time data of the patient against this digital model of a “healthy recovery path.” When the real patient begins to deviate from the model—even slightly—the dashboard flags a triage alert.
This shifts the clinical question from “What happened?” to “What is about to happen?” It allows care teams to administer antibiotics before a fever spikes, or adjust diuretics before fluid overload sends a heart failure patient back to the ER.
Read More: AI Clinical Workflows in Action: Real-World Examples of Human-AI Synergy
The Logistics of the “Rapid Response” Home
Predicting a problem is only half the battle; you must be able to solve it. When that dashboard turns Red, the logistics of the virtual hospital spring into action.
The response is tiered and immediate. First, the Command Center initiates a high-definition video consultation. This can happen through a tablet, a smartphone, or even the patient’s television. A physician can visually assess the patient, ask questions, and determine the severity of the situation within seconds of the alert.
If physical intervention is required, the system triggers automated dispatch protocols. Much like ride-sharing apps optimize driver routes, healthcare logistics platforms identify the nearest available mobile integrated health unit or home-care nurse.
GPS-optimized routing ensures that a clinician, oxygen delivery, or mobile imaging unit arrives at the patient’s door in the shortest possible time.
The loop is closed by the dashboard itself. Once the intervention is made—medication administered or therapy adjusted—the AI continues to track the patient’s response. Did the heart rate stabilize? Did oxygen levels return to baseline? If the data doesn’t show improvement, the escalation protocol continues, potentially leading to a traditional hospital transfer. But because of early intervention, these readmissions are significantly reduced.
The Human Element: Freedom Through Surveillance
Whenever we discuss continuous monitoring and AI, the conversation naturally turns to privacy. Is it invasive to be watched by an algorithm?
The reality of modern at-home care safeguards patient dignity. Unlike a camera in a hospital room that broadcasts a video feed, AI dashboards focus on data patterns. Ambient sensors can detect if a person has fallen in the bathroom using radar or lidar technology without ever capturing a visual image of the patient. The system is interested in the metrics of health, not the visual privacy of the home.
Paradoxically, this surveillance offers freedom. For patients, the psychological benefit of healing at home is immeasurable. They sleep better in their own beds, which is crucial for immune function. They eat familiar food, avoiding hospital malnutrition. The presence of pets and family members lowers cortisol levels and promotes healing.
For many high-risk patients, the fear of being “alone” during a medical crisis is paralyzing. Predictive safety nets remove this fear. Patients know they are being watched over by a team of experts 24/7, even if those experts aren’t physically in the room. This “freedom through surveillance” allows them to focus on recovery rather than anxiety.
Read More: The Hidden Risks of AI in Healthcare: Ensuring PHI Security Amid Data Explosion
Safety is a Signal, Not a Room
At Care Medicus, we believe the future of healthcare is moving home—and the momentum is undeniable. As rising costs, workforce shortages, and an aging population reshape the U.S. healthcare system, at-home care is becoming not just an alternative, but the new standard. Experts predict that within a decade, as much as half of today’s hospitalizations will take place in the comfort and safety of patients’ homes.
This shift is more than a trend. It represents a revolution in how we think about safety, triage, and care delivery. The home is becoming an extension of the hospital—smarter, connected, and supported by intelligent monitoring that makes high-quality care accessible to every community. Predictive analytics now allow us to detect issues early, intervene sooner, and deliver safer care without requiring four hospital walls.
Now is the time to embrace this transformation. Healthcare organizations must rethink how they deploy technology, support clinicians, and engage patients. The goal is no longer to build more beds—it’s to make the beds we already have smarter, safer, and part of a connected health ecosystem.
Partner with Care Medicus to lead the transition to home-based, predictive, technology-enabled care. Together, we can bring the future of healthcare into the place where patients heal best—home.






Leave a Reply